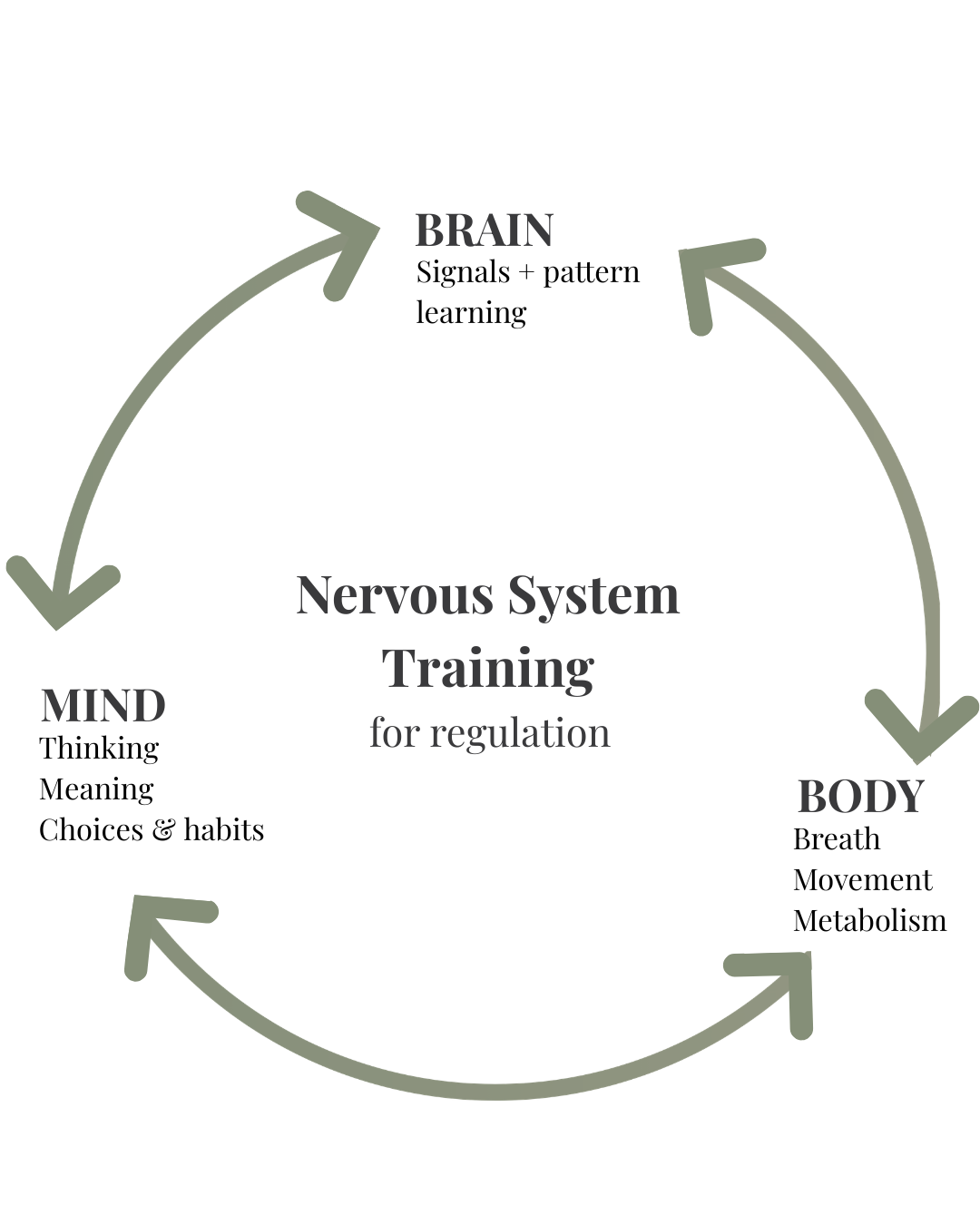
What You’ll Learn About How Stress Rewires Your Brain and Body
-
Why chronic stress rewires the brain and body through neuroplasticity, embedding survival-driven patterns that affect performance and recovery.
-
How stress changes brain function, from amygdala hyperactivity and reduced prefrontal control to memory and decision-making impairments.
-
The physical impact of stress, including chronic muscle tension, postural imbalances, shallow breathing, and heightened pain sensitivity.
-
Why these changes create a vicious cycle, keeping the nervous system locked in survival mode even when immediate stressors are gone.
-
How to retrain the brain and body using recovery practices, breathing retraining, and nervous system regulation strategies to restore clarity, resilience, and long-term performance.
A science-led guide for professionals who want to understand stress differently and turn nervous system insights into a performance advantage.
This post is part of a larger piece about nervous system training for stress and performance.
Click here for: The Complete Guide to Nervous System Training for Stress and Performance
How Stress Rewires Your Brain and Body: Why It Becomes a Cycle
The Altered Baseline: From Balance to Chronic Stress Mode
Your nervous system is built to rebalance after stress, but chronic demands can shift its operating baseline. Under prolonged workload, unresolved adversity, or environmental pressure, temporary stress responses become embedded as the “new normal.” For efficiency, your brain begins to issue automatic instructions that keep you primed and ready for stress, even if these instructions undermine long-term health and performance.
The result is a nervous system constantly operating in a low-level survival mode, becoming hyper-vigilant, tense, and less flexible. This is what can give rise to unwanted symptoms such as poor sleep, a persistent feeling of stress or inability to relax, lack of concentration and an impaired ability to enter into a recovery state.
How Past Stress Shapes Present Performance
Your brain and nervous system do not respond to the present moment in isolation. Every reaction is influenced by prior experience, and much of what the brain retains comes from its constant two-way communication with the body. This ongoing feedback loop keeps you adaptive to changing circumstances, and you learn from this. Not all memory is conscious; past stress exposures, patterns of muscle use, relationships and the environments you’ve operated in leave imprints that guide how your body/mind system adapts today.
In this way, the brain makes current predictions based on current information plus past learning, drawing on historical templates and patterns of reactivity to anticipate and prepare for what might come next with utmost efficiency. While this ensures rapid and efficient reactions, it also means that outdated or stress-driven patterns can continue to shape our behaviour even when they are not the best fit for current circumstances.
Through neuroplasticity, stress rewires the nervous system. What begins as short-term adaptation becomes a learned state of survival. Unless new and consistent feedback signals are introduced that demonstrate that the needs of the environment have changed, the brain will continue operating in this stress-shaped mode.
Why Your Brain Becomes More Threat Sensitive Under Stress
When stress is frequent or prolonged, the brain adapts by becoming more efficient at detecting and responding to potential danger. A bit like over training one set of muscles over another, chronic and overwhelming stress trains your brain and rewires your threat detection system for increased threat sensitivity. This shift is protective in the short term but can become maladaptive when it persists.
Amygdala Hyperactivity: The Brain’s Overactive Alarm System
The amygdala, the brain’s primary threat-detection centre, becomes increasingly reactive under repeated stress. It begins to interpret neutral or ambiguous cues as signals of danger, keeping the system on high alert. This part of the brain is feeling based, rather than responsive to words, so it needs physiological shifts towards parasympathetic activity to calm its overactive bias towards threat detection. A cognitive shift in mindset alone won’t be enough to calm that part of the brain.
Reduced Prefrontal Control and Decision-Making Under Stress
The prefrontal cortex, which usually provides perspective and helps calm fear responses, loses influence during chronic stress. As a result, rational appraisal and decision-making are more easily overridden by automatic survival reactions.
Stress Hormones and the Brain: Cortisol’s Impact on Learning and Memory
Elevated cortisol and other stress hormones feed back into the brain, reinforcing amygdala sensitivity and reducing plasticity in the hippocampus (involved in memory and context). This creates a cycle where the brain expects threat, perceives it more readily, and encodes stress-based patterns more deeply.
In effect, the brain recalibrates toward vigilance. What once required genuine danger to trigger now happens automatically, embedding a state of hyper-sensitivity to stress.
Chronic Muscle Tension: How Stress Shapes Posture and Pain
One of the most immediate ways the brain encodes stress is through our muscles. Chronic stress always comes with a muscular counterpart. Tension in the shoulders, neck, or jaw is not just a habit; it is the result of neural circuits maintaining muscle activation over time. Stress activates muscle tension in order to facilitate action. Chronic stress trains the body to be prepared for action at all times and keeps the brain sending signals to tighten those muscles.
- Muscle Memory
Repeated contractions or postures are stored as motor memory within the brain. If contraction signals are sent consistently, the muscles adapt by retaining this tension even in the absence of immediate stress. This is why people often find themselves holding their shoulders up or clenching their jaw unconsciously. - The Gamma Loop
The gamma loop is a sensorimotor feedback mechanism involving the spinal cord and brain that fine-tunes muscle tone and proprioception. Under chronic stress, repeated contraction signals can raise the baseline level of tension within this loop. Over time, the nervous system recalibrates, perceiving this elevated state as “normal.” - Stress and Pain Sensitisation
Prolonged activation of the stress response maintains muscle contraction and increases the sensitivity of pain pathways. This reinforces tightness and contributes to chronic pain conditions, making recovery more difficult without active retraining of the body–brain connection.
Stress and Breathing Patterns: From Shallow Breathing to Recovery
Optimal Breathing at Rest
Under ideal conditions, healthy breathing occurs at a steady rhythm of around 5–6 breaths per minute. This involves full rib cage expansion and effective diaphragm movement, allowing gas exchange to take place deep in the lungs where oxygen uptake is most efficient. In this state, oxygen is absorbed, carbon dioxide (CO₂) is exhaled, and crucially, enough CO₂ is retained in the bloodstream to optimise the release of oxygen from haemoglobin to tissues.
Stress-Induced Breathing Shifts
When the body perceives stress, the brain rapidly adjusts breathing patterns to prepare for action. Heart rate rises, breathing becomes faster and shallower, and ventilation is directed higher into the chest rather than deep into the lungs. While adaptive in short bursts, chronic stress teaches the nervous system to maintain this altered pattern. Over time, shallow, rapid breathing becomes the new baseline, a form of habitual hyperventilation.
Biochemical Consequences
Breathing is regulated primarily by CO₂, not oxygen. Rising CO₂ levels are what trigger the body’s urge to breathe. Under shallow, rapid breathing, CO₂ is excessively exhaled, lowering blood levels below optimal. The brain gradually recalibrates, treating this low-CO₂ state as “normal.” As a result, breathing is triggered prematurely, independent of true oxygen demand. This creates a self-reinforcing cycle: stress drives shallow breathing, and shallow breathing further maintains the stress response.
Muscular Restrictions
Stress also increases muscular tension. The diaphragm and intercostal muscles, essential for deep, efficient breathing, become restricted. Instead of allowing full breath expansion, they limit depth and expansion, reinforcing the shallow, rapid pattern. Over time, this contributes to postural imbalances, fatigue, and reduced breathing efficiency.
Performance and Recovery Implications
A chronically shallow breathing pattern has wide-ranging consequences. It:
- Sustains low-level stress and anxiety.
- Reduces oxygen delivery to tissues and the brain.
- Contributes to musculoskeletal problems such as back and shoulder pain.
- Weakens immune function.
- Promotes fatigue and reduced recovery capacity.
When breathing is re-trained it involves re-educating the brain about how to accept higher levels of CO2. When this happens, breathing can once again slow and deepen in alignment with parasympathetic activity. This shift restores efficient oxygen delivery, calms the stress response, and enhances both performance and recovery.
INTERESTED IN TRAINING 1:1 IN FUNCTIONAL BREATHING? SEE THE FUNCTIONAL BREATHING COURSE HERE
To understand why these changes happen below conscious awareness, see Your Brain on Stress: Conscious vs. Unconscious Agendas
In Summary:
How Stress Rewires the Brain and Body and How to Retrain It
Chronic stress rewires your brain and body, embedding survival-driven patterns that compromise decision-making, recovery, and performance. What begins as short-term adaptation, muscle tension, shallow breathing, heightened vigilance becomes a default operating mode, even when the original stressors are no longer present. Your brain, designed for efficiency, continues to issue survival-driven instructions that keep you primed for action but undermine long-term recovery and performance.
The good news is that these patterns are not fixed. Thanks to neuroplasticity, the same processes that embed stress can also be harnessed to recalibrate and retrain the system. By introducing new, consistent feedback from your body into your brain, through targeted recovery practices, physiological retraining, and technologies that support optimal function, the nervous system can learn to shift out of survival mode and back into balanced regulation.
The opportunity is to actively re-train your brain, which can be done directly with technologies like neurofeedback, alongside reclaiming your cardiovascular fitness, strength and mobility and breathing capacity, CO2 tolerance and oxygenation. By supporting your brain and body to relinquish survival patterns, performance, resilience, and recovery support each other. When your nervous system is recalibrated, your body returns to a better balance point, your mind can naturally arise out of a stable physical environment, and you regain your capacity to perform at a high level without sacrificing long-term wellbeing.
About BodyMindBrain:
At BodyMindBrain, we help motivated adults with high-demand lives build strength, energy, and resilience by training the body, brain, and mind as one integrated system.